PDF-AJNR12 MayfJune 1991
Author : linda | Published Date : 2022-09-06
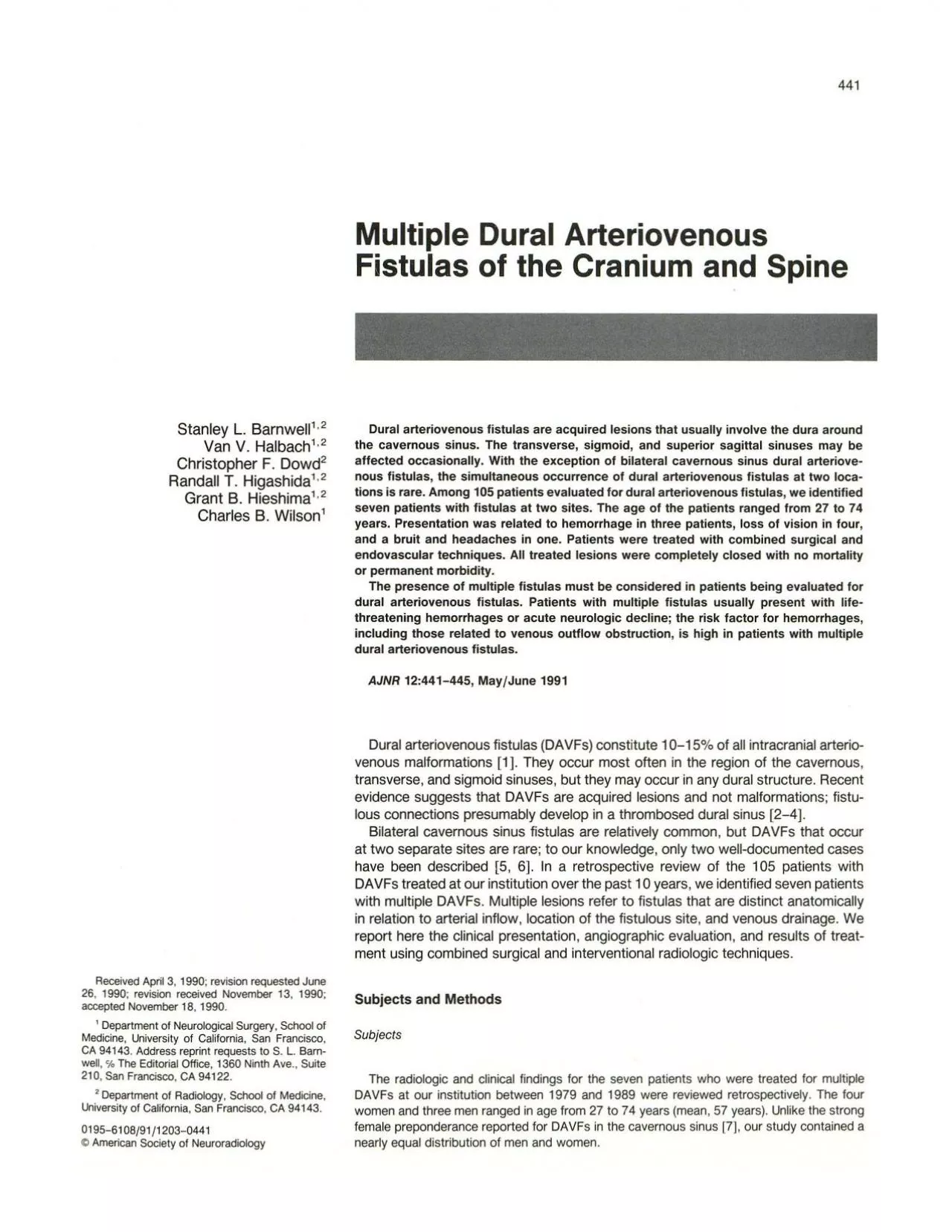
MULTIPLE DURAL ARTERIOVENOUS FISTULAS 445 A B Fig 6Patient 7 Fig 5Patient 6 Right external carotid artery injection lateral projection shows two fistulas one involving
Presentation Embed Code
Download Presentation
Download Presentation The PPT/PDF document "AJNR12 MayfJune 1991" is the property of its rightful owner. Permission is granted to download and print the materials on this website for personal, non-commercial use only, and to display it on your personal computer provided you do not modify the materials and that you retain all copyright notices contained in the materials. By downloading content from our website, you accept the terms of this agreement.
AJNR12 MayfJune 1991: Transcript
Download Rules Of Document
"AJNR12 MayfJune 1991"The content belongs to its owner. You may download and print it for personal use, without modification, and keep all copyright notices. By downloading, you agree to these terms.
Related Documents