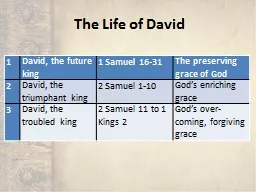
PPT-Pink / Pediatrics Primary Author: Dr. David Saquet
Author : olivia-moreira | Published Date : 2019-11-20
Pink Pediatrics Primary Author Dr David Saquet 2019 Protocol Update The Big Picture The biggest change for the pediatric protocol section is the decrease of pediatric
Presentation Embed Code
Download Presentation
Download Presentation The PPT/PDF document "Pink / Pediatrics Primary Author: Dr. Da..." is the property of its rightful owner. Permission is granted to download and print the materials on this website for personal, non-commercial use only, and to display it on your personal computer provided you do not modify the materials and that you retain all copyright notices contained in the materials. By downloading content from our website, you accept the terms of this agreement.
Pink / Pediatrics Primary Author: Dr. David Saquet: Transcript
Download Rules Of Document
"Pink / Pediatrics Primary Author: Dr. David Saquet"The content belongs to its owner. You may download and print it for personal use, without modification, and keep all copyright notices. By downloading, you agree to these terms.
Related Documents