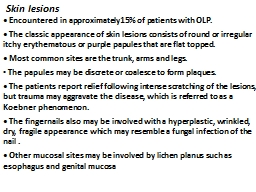
PPT-Skin lesions • Encountered in approximately15% of patients with OLP.
Author : melanie | Published Date : 2024-02-09
The classic appearance of skin lesions consists of round or irregular itchy erythematous or purple papules that are flat topped Most common sites are the trunk
Presentation Embed Code
Download Presentation
Download Presentation The PPT/PDF document "Skin lesions • Encountered in approxi..." is the property of its rightful owner. Permission is granted to download and print the materials on this website for personal, non-commercial use only, and to display it on your personal computer provided you do not modify the materials and that you retain all copyright notices contained in the materials. By downloading content from our website, you accept the terms of this agreement.
Skin lesions • Encountered in approximately15% of patients with OLP.: Transcript
The classic appearance of skin lesions consists of round or irregular itchy erythematous or purple papules that are flat topped Most common sites are the trunk arms and legs The papules may be discrete or coalesce to form plaques . LANGERHANS CELL HISTIOCYTOSIS. . Letterer-. Siwe. disease. . Hand-. Schuller. -Christian disease. . . Eosinophilic. . granuloma. . Congenital self-healing . reticulohistiocytosis. (Hashimoto-. Pritzker. by. Murat . Sensoy. , . Geeth. de Mel, . Wamberto. . Vasconcelos. . and Timothy J. Norman. Computing Science, University of Aberdeen, UK. 1. Outline. Introduction. Motivation. OLP Architecture. A Case Study and Performance. Dr. . S.Anandan. , . Dean & Professor of Dermatology. SRMC & RI, . Porur. , Chennai – 600 116. OBJECTIVES. Introduction . Pathogenesis. Heat shock protein in OLP.. Types of OLP. Treatment modalities. axial . Spondyloarthritis:. when . to . repeat an MRI?. R. . Sengupta. * . 1. , H. Marzo Ortega. 2,3. , D. McGonagle. 2,3. , A. Bennett. 4. 1. Royal National Hospital for Rheumatic Diseases, Bath; . Skin pathology Skin diseases are common and diverse, ranging from irritating acne to life-threatening melanoma. Either intrinsic to skin, or systemic diseases involving many tissues, or genetic syndromes such as neurofibromatosis. Site. . Name. . Scalp. . Tinea. . capitis. . Feet. . Tinea. . pedis. . Groin. . Tinea. . cruris. . Body. . Tinea. . corporis. . Nails. . Tinea. . unguium. . (. onychomycosis. ESULTS Although identifying populations of alien species of concern wa giant toad, cane toad, bufo toad, bufo L** L - Chamaeleonidae Chamaeleo jacksonii xantholophus Jackson's chameleon N** N Skin tags. (. acrochordon. ). common benign outgrowths of skin affect mainly the middle-aged and elderly. .. Skin tags are soft skin-. coloured. or pigmented pedunculated papules commonly found around the neck and within the major . dermoscopic. images is crucial and results in an increase in the survival rate. The clinical ABCD (asymmetry, border irregularity, color variation and diameter greater than 6mm) rule is one of the most widely used methods for early melanoma recognition. However, accurate classification of melanoma is still extremely difficult due to following reasons(not limited to): great visual resemblance between melanoma and non-melanoma skin lesions, less contrast difference between skin and the lesions etc. There is an ever-growing need of correct and reliable detection of skin cancers. Advances in the field of deep learning deems it perfect for the task of automatic detection and is very useful to pathologists as they aid them in terms of efficiency and accuracy. . . Hasan. M.B.CH.B. C.A.B.S-D.V. Psoriasis is a chronic, non-infectious, inflammatory skin disorder, characterized by well-defined . salmonpink. . plaques bearing large adherent silvery centrally attached scales.. HISTORY. EXAMINATION. TOOLS. TESTS. Clinical Dermatology. Visual . Speciality. History. History . of present skin condition. Duration, Site . at onset, details of . spread, Itch, Burning. Wet, dry, . planus. . pityriasis. . rubra. . pilaris. Erythroderma. . . Papulosquamous. disorders. may . be caused by reactivation of either human herpes virus 7 or . 6.. The . disease seems . not to be . General points in presentation. Skin tumors are the most common body tumors .. Most skin lesions presented by patients are benign; however, some concern has caused the patient to make an inquiry, and a correct diagnosis is important. . •Hyperkeratosis: Increased production of keratin. . •. Acanthosis. : An abnormal but benign thickening of stratum . spinosum. . . •Intra and extracellular accumulation of fluid in the epithelium .
Download Document
Here is the link to download the presentation.
"Skin lesions • Encountered in approximately15% of patients with OLP."The content belongs to its owner. You may download and print it for personal use, without modification, and keep all copyright notices. By downloading, you agree to these terms.
Related Documents