PDF-A- and V-Patterns and Oblique Muscle Overaction
Author : olivia-moreira | Published Date : 2015-09-13
18 A and VPatterns Clinical Features Etiology Management with Horizontal Rectus Muscle Offsets Inferior Oblique Overaction Etiology Clinical Features Differential
Presentation Embed Code
Download Presentation
Download Presentation The PPT/PDF document "A- and V-Patterns and Oblique Muscle Ove..." is the property of its rightful owner. Permission is granted to download and print the materials on this website for personal, non-commercial use only, and to display it on your personal computer provided you do not modify the materials and that you retain all copyright notices contained in the materials. By downloading content from our website, you accept the terms of this agreement.
A- and V-Patterns and Oblique Muscle Overaction: Transcript
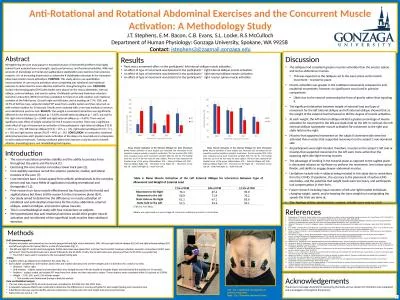
18 A and VPatterns Clinical Features Etiology Management with Horizontal Rectus Muscle Offsets Inferior Oblique Overaction Etiology Clinical Features Differential Diagnosis Management Superior Obliq. Pictorial Drawing. 2D illustration of a 3D object. Shows three faces of an object in one view. Provides a realistic view of an object. Three types. Isometric. Oblique (Cavalier. ). Perspective. Oblique (Cabinet). Research Planning, . Inc. May . 1, . 2012. ESI workshop, Mobile Alabama. Outline. ESI concept. Current production process. Challenges. Relevant programs and standards. Core Concepts. A consistent classification of shoreline morphology / habitat. Vijit. Chouhan. 1. , Akin Cil. 1,2. , James Barnes. 1,2. 1. UMKC School of Medicine, . 2. Truman Medical Center. INTRODUCTION. The annular ligament is a complex structure in the elbow that assists in stabilization of the elbow joint. . Chitraka. . Wickramarachchi. Dr. Blair Robertson. Dr. Marco . Reale. Dr. Chris Price. Prof. Jennifer Brown. Introduction. Literature Review. Methodology. Results and Discussion. Outline of the Presentation. . and. TUCKING. . of INFERIOR OBLIQUE MUSCLE. DURANOGLU Yasar; . MD. Akdeniz . University. . Medical. . School. . Department. of . Ophthalmology. Antalya/TURKEY. 2012. . . The . inferior oblique muscle . DR.PREM CHAND PALADUGU . AARUPADAI VEEDU MEDICAL COLLEGE & HOSPITAL . DEFINITION. : A CLINICAL CONDITION CHARACTERISED BY SEVERE RESTRICTION OF ACTIVE & PASSIVE MOTION OF GLENOHUMERAL JOINT AND IN WHICH NO OTHER CAUSE CAN BE DOCUMENTED. Suh. , . Soh. . Youn. , et al. "Extraocular Muscle Compartments in Superior Oblique . PalsyMuscle. Compartments in Superior Oblique Palsy." . Investigative ophthalmology & visual science. 57.13 (2016): 5535-5540.. Gasquet. Module 1: Abdominaux. Plan du cours. Introduction:. Présentation Dresse de . gasquet. Approche . apor. Objectif de la méthode. Anatomie:. Muscles abdominaux. Muscle diaphragme. Les trois notions de base. Oblique Flankplasty as an Alternative to Lower Body Lift Dennis J. Hurwitz, M.D., FACS Director of the Hurwitz Center for Plastic Surgery Clinical Professor Of Plastic Surgery Disclosure Comprehensive Body Contouring diplopia. Teaching . VideoImages. Neurology. Resident and Fellow Section. © . 2015 . American Academy of Neurology. Vignette. 63-year-old patient. Admitted . for acute ataxia and binocular oblique . X-eye SF160FCT-ray 3D CT Analysis160kV Micro-focus X-ray Open Tube with 09 micron focal spot size460mm x 510mm Table Size with full enhanced stroke axis XYZTR Max magnification up to 4800xUnparallel uas. data. Sabina Bastias and . Kellyn. Montgomery. GIS595/MEA592 Spring 2018. UAS Mapping for 3D Modeling. Background. Radial distortion. Mitigated through software correction (Brown’s distortion model). Exercising the core muscles can reduce lower back pain (2). . Core stability exercises recruit the anterior, posterior, medial, and lateral muscles of the core (7).. Core exercises have a broad appeal from athletic professionals to the everyday person and has many fields of application including recreational and therapeutic (1,3).. . features. .. Structure . of heart wall, myocardium, . valves. , . anuli. fibrosi . Dr. Altdorfer. Structure of heart . wall. Pericardal. . sack. Epicardium. Pericardium. Fibrous. . skeleton. (.
Download Document
Here is the link to download the presentation.
"A- and V-Patterns and Oblique Muscle Overaction"The content belongs to its owner. You may download and print it for personal use, without modification, and keep all copyright notices. By downloading, you agree to these terms.
Related Documents